MITRAL STENOSIS:
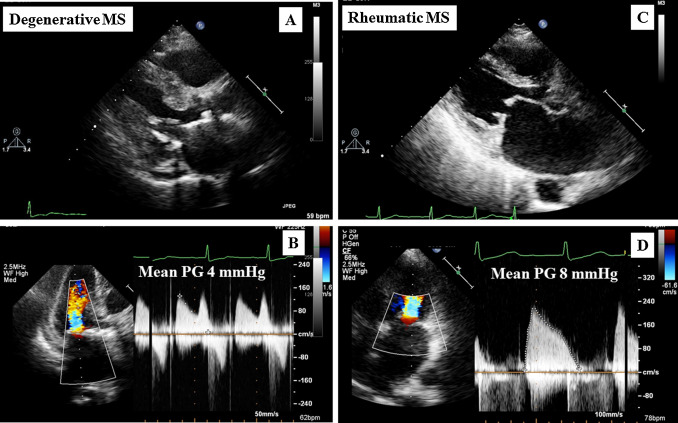
A narrowing/thickening/obstruction of the mitral valve that impedes diastolic flow traveling from Left Atrium to Left Ventricle.
MURMUR: low-pitched, diastolic rumble w/an opening snap
CAUSES:
- Rheumatic fever, severe annular calcification that interferes w/function of MV leaflets, congenital such as atresia (absence of a normal opening) or parachute (only 1 papillary muscle attached to the MV creating a parachute appearance)
- Secondary due to left atrial mass/tumor or MV vegetation, prosthetic valve dysfunction, radiation, autoimmune disease.
COMPLICATIONS:
- Increased LA pressure
- MV leaflet doming
- LA enlargement
- possible a-fib >backup and enlargement of Pulmonary Veins
- increased pulmonary artery pressure
- Pulmonary Hypertension
- increased RV and RA pressure
- right heart enlargement
- Tricuspid Rregurgitation
- IVC dilation and SVC dilation
- hepatic and jugular vein dilation
- systemic vein dilation
- ascites (accumulation of fluid)
- ankle swelling.
SIGNS AND SYMPTOMS
- Chest pain, coughing, dizziness, dyspnea, fatigue, heart palpitations, hemoptysis, irregular rhythms, murmur, right heart failure, shortness of breath, swollen feet, symptoms of stroke, syncope.
TREATMENT:
- Mitral balloon valvotomy, valvuloplasty, mitral valve replacement.
2D ECHO
- Diastolic doming of AMVL creates a hockey stick appearance. MV thickening more than >3mm
- Decreased MVA. Planimetry rage: 4-5 cm2, most patients are asymptomatic if MVA less than <1.5cm2.
- PSAX, Zoom, enhance, avoid excessive gain, 3 + beats average.
- Anterior motion of the PMVL due to stenosis and tethering.
- Commissural fusion – contributes to doming effect.
- Thickening and fibrosis.
- LA pressure increase causing LA enlargement, possible LA spontaneous echo contrast (smoke)
- Dilated RA, SVC, IVC and hepatic vein. Watch for IVC collapse, IVC normal range, and hep vein.
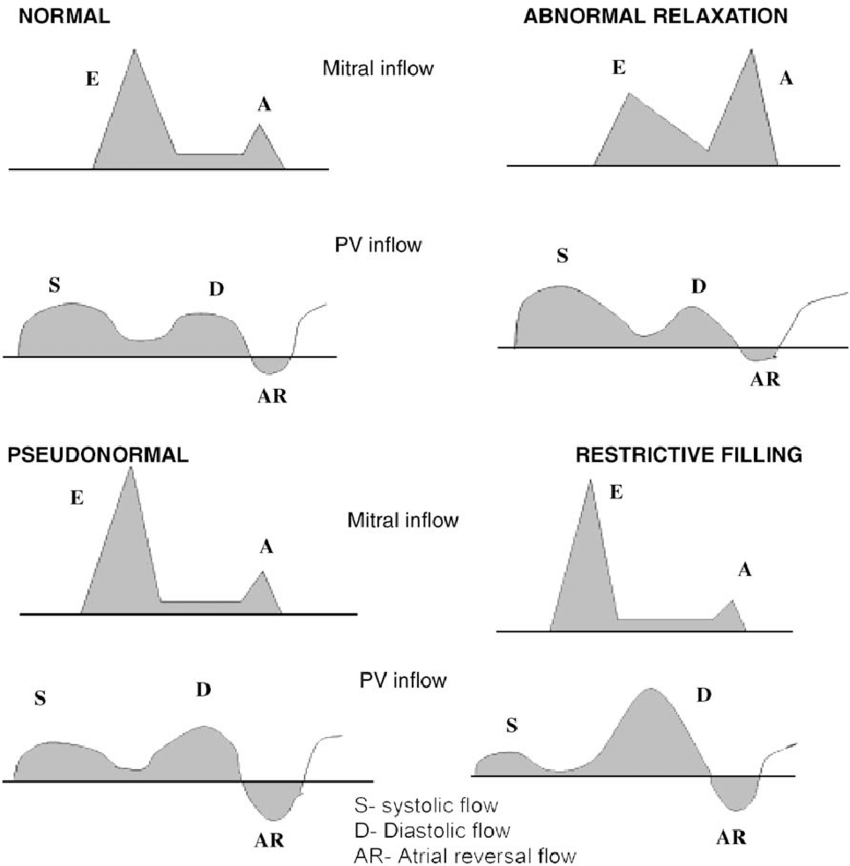
- M-mode: decreased EF slope 0-30mm/s, reduced amplitude of E wave, decreased/absent A wave-> CWD Doppler.
- MS severity is usually determined by the pressure half time (p1/2t), MVArea and PG, and PISA – proximal isovelocity Surface Area.
MV annulus diameter at mid diastole
MVA= 220/pressure half-time
Normal 30-60,
Mild 90-150,
Moderate 150-219,
Severe >220
DT Method & MVA: P1/2t = DR x 0.29 and MVA = 759/DT
- PTH – forces RV to work harder = ventricular hypertrophy. Increased RV pressure flattens interventricular septum. SAX view – paradoxical aka parallel wall motion, D-shaped LV in diastole and systole.
- Pulmonary Valve mid-systolic closure creates a flying W.
MITRAL REGURGITATION:
Mitral valve consists of several components:
- LA wall, Mitral annulus, anterior and posterior leaflets, chordae, papillary muscles, LV myocardium underlying the papillary muscles.
- Dysfunction of any of these can result in MR.
- Mitral annular dilation is associated with either LA or LV dilation nd results in MR. the annulus is smaller in sytole than in diastole. Impaired annulus w/mitral calcification impairs systolic contraction. Short-axis views, the annular calcium may be focal or extensive.
- Diseases: myxomatous disease, rheumatic disease, endocarditis, Marfan syndrome.
- Myxomatous disease: characterized by thickened, redundant leaflets and chordae w/excessive motion and sagging of portions of the leaflets into LA in systole.
- Chordial disruption or elongation lead to MR because of inadequate tensile support of the closed leaflets. Severe bowing of the leaflet, directed to ventricular apex.
- Rheumatic MR: commissural fusion, chordial fusion and shortening are more prominent.
- Endocarditis: leaflet disruption, perforation or deformity.
- MARFAN SYNDROME: assoc w/long, redundant anterior leaflet that sags into the LA in systole.
- Age-related degenerative changes: irregular areas of thickening and increased echogenity.
- ISCHEMIC: due to regional LV dysfunction and abnormal contraction. MI patients: results in MR at rest. Normal patients: ischemia w/stress, intermittent MR.
RESPONSE OF THE LEFT VENTRICLE, LEFT ATRIUM, AND PULMONARY VASCULATURE
- MR results in LV volume overload because the stroke volume increases as blood is ejected both forward into the aorta and retrograde across the MV.
- Acute MR, LV empies moe completely, EF increases. Regurgitant volume is delivered into a small, noncompliant LA, resulting in a significant increase in pressure and v-wave in LA pressure curve.
- Chronic MR, LV diastolic volume increases and EF is normal range or mildly incrased. Afterload Is normal and EF typically is in the normal range. Look at LV size – important. Progressive LV dilation occurs, SV increases. Irreversavle contractility can occur w/o symptoms. LA gradually dilates, maintaining normal pressure.
- Afterload may decrease in MR due to ejection into the low-pressure LA.
- Pulmonary artery pressure increases passively In response to both the chronic, mildly elevated LA pressure. When pressure is evelated, pulmonary vascular resistance increases.
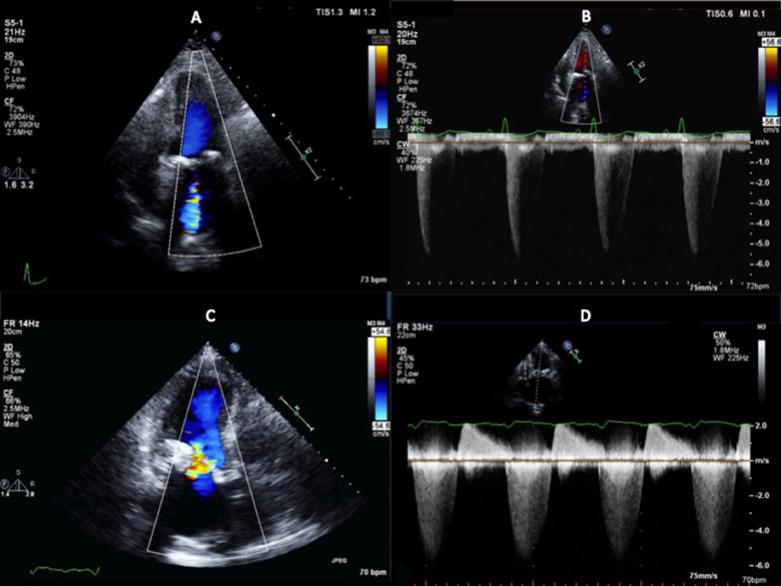
2D ECHO:
- Color flow imaging, CW Doppler. Color Doppler allows for detection of the presence of MR and separates mild regurgitation from moderate to severe disease. Shape and direction of the jet is helpful.
- Dilation of LV and mitral annulus results in central, symmetric regurgitant jet.
- PLAX, PSAX, A4 and A3 aka long axis are useful
- Central jet w/area less than 4 cm2 or less than 20% of the LA area in a nonoblique view is – mild MR.
- CW Doppler spectral recording – shows rapid increase in velocity in isovolumetric contraction (proportional to the rate of rise in LV pressure of dP/dt) from baseline to a max velocity of 5 to 6 m/s. Velocity stays high throughout the systole. During ISVR – the velocity rapidly returns to baseline.
- Acute MR: increase in LA pressure during late systole – a v-wave – usually is present because of a steep pressure-volume relationship of the nondilated LA. Pressure gradient between LA and LV is high.
Vena Contracta:
- Diameter should be measured if color Doppler imaging shows an eccentric or large jet or if CW Doppler suggests more than mild MR.
- Mild MR: VC is visualized in PLAX or PSAX, Apical views may be used If those other 2 aren’t visualized.
- Measurements made with:
- Transthoracic parasternal or TEE 120* long-axis view
- Visualization of the narrow neck between the proximal acceleration and distal jet expansion
- Zoom mode
- Measurement perpendicular to the direction of flow.
- Vena contracta of more than 0.3cm indicates further quantification of regurgitant severity needed.
PROXIMAL ISOVELOCITY SURFACE AREA – PISA
Measurements requirements:
- A4C or PLAX
- Narrow sector width
- Zoom mode
- Aliasing velocity set at 30 to 40 cm/s in the direction of blood flow
- Simulation 2D imaging to show leaflet closure plane
- Radius measured from aliasing velocity to valve closure plane
- Underestimation of regurgitation – PISA occurs flattened
PISA = 2 x pi x r2 Regurgitant flow= 2 x pi x r2 x Va (Aliasing velocity at radial distance)
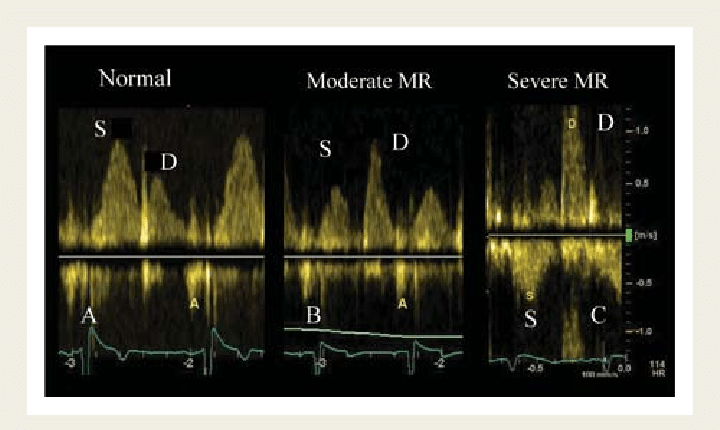
PULMONARY VEIN FLOW REVERSAL
- Systolic flow can be seen in some patients. A4C views. TEE helpful w/eccentric flow.
- False-negative results occur when LA is severely enlarged and compliant
- False-negative also seen in patients in irregular sinus rhythm.
Works Cited
Full Information on Mitral Stenosis can be found in Susan DeWitt: “Echocardiography from Sonographer’s Perspective” at http://www.echonotebook.com/
and Catherine M. Otto “Textbook of Clinical Echocardiography” at https://www.elsevier.com/books/textbook-of-clinical-echocardiography/otto/978-0-323-48048-2

